

If you are experiencing pain and swelling in your eye, call Center for Sight immediately as these could be a sign that another surgery may be warranted. You will need to schedule and keep follow-up appointments to ensure the procedure was successful and you are not experiencing any side effects. Many people experience results immediately following their procedure, but it could take a few days for your vision to return to normal.
#Retina reattachment surgery how to#
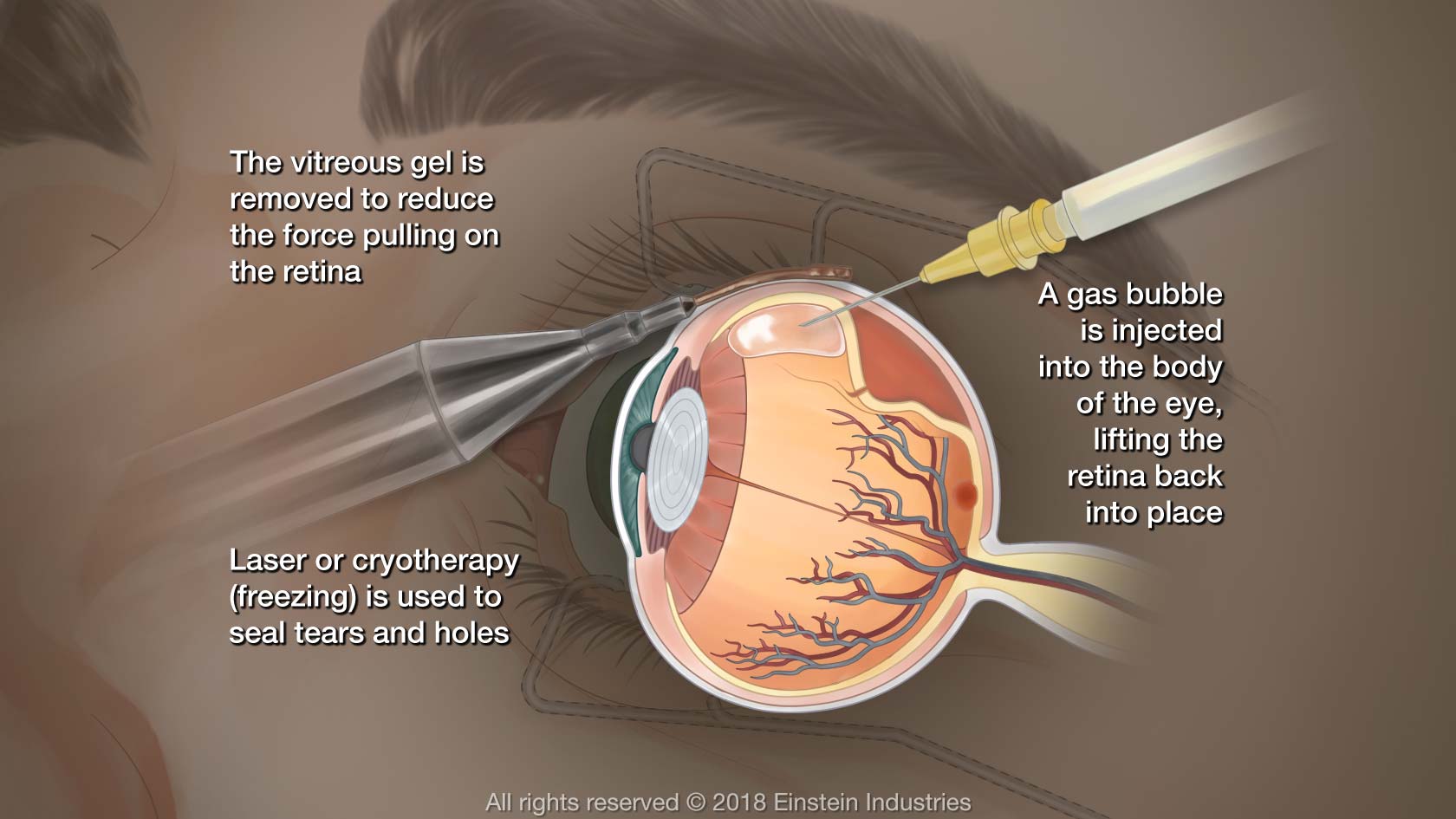
They will provide very specific instructions about how to position your head after the procedure for up to eight hours following the procedure this allows the gas bubble they injected to stay in the right place until the retina has healed enough to hold itself in the proper position. The most important thing to remember following a retinal detachment surgery is to listen to your doctor’s instructions about positioning.
#Retina reattachment surgery Patch#
Recoveryįollowing your procedure, you will be asked to wear an eye patch and your physician will prescribe medication to ensure you do not experience too much pain. Reattachment procedures generally take between one to two hours, depending on the technique being used, so you can expect to be out and home on the same day as your surgery. This procedure requires your doctor to remove some of the vitreous humor from inside of your eye.ĭuring the procedure, local anesthesia will be used to ensure you feel minimal pain during the surgery. In very severe cases of retinal detachment, a procedure called a vitrectomy may need to be performed. Once the detached portion of your retina is properly positioned, a cryogenic device will be used to seal the retina in place at the back of your eye. The type of surgery your surgeon recommends will depend on several factors, including how severe the detachment is. Your physician will position this expanding bubble in such a way as to make it “float” on top of the detached retina, pushing it back into place. If your retina has detached, youll need surgery to repair it, preferably within days of a diagnosis. What to Expectĭuring retinal detachment surgery, your physician will inject an expanding bubble of gas into your eye. RisksĬenter for Sight’s retina specialist will discuss the complications and risks with your prior to any procedures. Most detachments can be repaired via a single surgery, but in some cases, people may require more than one procedure to fully repair the damage. The good news is that retinal detachment surgery is considered safe and has very positive long-term outcomes.

While some cases can be treated non-surgically, the most common treatment for a detached retina is surgery. These include among other things, having pre-existing eye conditions like nearsightedness or uveitis, or having undergone eye surgery previously. There are a host of risk factors that make it significantly more likely that you will suffer a retinal detachment at some point in your life. If left untreated, a retinal detachment can lead to permanent vision loss, so it requires immediate medical treatment. Generally, the retina loses its oxygen supply because of a tear or total detachment from the back of the eyeball. As the retina loses oxygen, it becomes very difficult, if not impossible, for the retina to process light impulses into visual images, ultimately blurring or blocking vision. Retinal detachment is a very serious medical condition that occurs when the retina is physically damaged to the point that it stops receiving the oxygen it needs to stay functional. This captured light is then transmitted through the optic nerve to the brain, where it is translated into the images we see. However, Arruga's ring suture method induced cataract more frequently than did other surgical procedures.The retina is a thin layer of cells positioned at the back of the eyeball that houses millions of light-sensitive nerve cells called ganglion, which absorb light focused on them by the cornea and the inner lens of the eye. There was no difference in postoperative ocular findings between only diathermy and combination of diathermy with segmental scleral-buckling procedures. Macular degeneration was caused or accelerated by detachment of the macula. This atrophy seems to be related to the long duration of retinal detachment before and after operation, which may cause malnutrition of the detached retina and result in incomplete recovery of visual cells, leading to chorioretinal atrophy. Chorioretinal atrophy with blackish pigment spots developed in the reattached retina a long time after surgery and caused defects in the visual fields. The most frequent causes of this fall in visual acuity after surgery were cataract and macular degeneration. The visual acuity had decreased in many patients. The average age was 35 years at the time of surgery and the average interval between the operation and this follow-up examination was 16 years. Patients treated successfully with retinal detachment surgery 11-39 years earlier were called back and examined. The goal of surgery is to reattach the retina to the back of the eye as soon as possible so that the blood supply can be reestablished.


 0 kommentar(er)
0 kommentar(er)
